Dr Helen Green and Dr Elizabeth Goulding accept referrals for gynaecological cancers, pre-cancers and complex benign gynaecological conditions.
Their interests in general gynaecology include complex surgical cases; minimally invasive surgery; vulval, vaginal and cervical dysplasia.
Dr Green and Dr Goulding are committed to providing state of the art and evidence-based care to their patients. Together they have created the Grace Gynaeoncology Group, the largest private Gynaecological Oncology centre on the Gold Coast, and the only service offering its patients a private multidisciplinary meeting to ensure the highest quality of care is delivered to every patient.
COMMON REFERRALS INCLUDE:
The most common reasons you may be referred to see Dr Goulding and Dr Green at Grace Gynaecology Group are listed below:
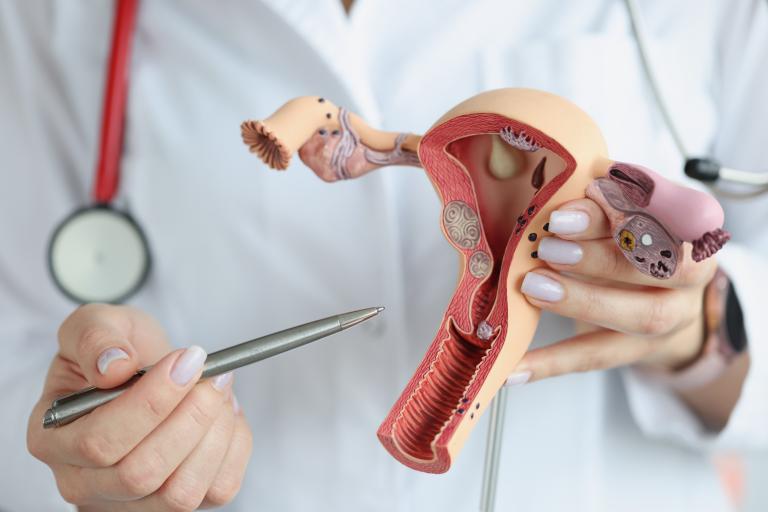
Gynaecological cancers require immediate, specialised treatment.
If you have a suspected or confirmed gynaecological cancer or pre-cancer, our doctors will see you promptly, with the aim of commencing treatment as soon as possible. They work closely with medical oncologists and radiation oncologists to ensure that efficient, high-quality, multidisciplinary care is available to all women with cancers involving the reproductive system.

When one or more of your family members have been diagnosed with cancer, it is advisable to investigate the implications for yourself and other close family members. In this case, your GP or a genetic specialist can talk to you about the likely risk of cancer in your family. In certain circumstances, you may be eligible to undergo genetic testing to help determine your risk. If you are estimated to have a higher risk of developing a gynaecological cancer, Dr Goulding and Dr Green can discuss the options to reduce your risk (these may include minimally invasive surgery).
If you have a personal history of breast cancer, you may also be referred to discuss the options to reduce your risk of other cancers or the options for hormonal manipulation to reduce your risk of breast cancer recurrence.

Abnormal uterine bleeding is defined as very heavy or longer than usual menstrual bleeding. It can also mean bleeding that does not follow a normal pattern, such as lighter bleeding between periods, bleeding after intercourse or bleeding after menopause.
There are many conditions that result in abnormal uterine bleeding, so a diagnosis may require various tests. An ultrasound can be very useful first step to determine the appropriate sequence of investigations and treatment options. Another useful investigation is a biopsy from the lining of the uterus (endometrium). This can diagnose many causes of abnormal uterine bleeding and help guide your treatment. If a biopsy is required, Dr Green and Dr Goulding can often perform this procedure during your appointment in their consulting suites, and if not have rapid access to a biopsy under a general anaesthetic (via a hysteroscopy, dilation and curettage).
Treatment options for abnormal uterine bleeding include non-surgical and surgical options. When surgical treatment is appropriate, minimally invasive surgery (including minimally invasive hysterectomy) is often possible.

The cervical screening program uses a combination of the new HPV test and the pap test (also called pap smear) to detect HPV infection and/or abnormal cells on the cervix that may lead to cervical cancer if untreated. We understand that an abnormal cervical screening result can be very stressful, however, it only rarely means that cervical cancer is already present.
If your results require specialist assessment, your GP will refer you for a colposcopy, which can be performed in Dr Green and Dr Goulding’s consulting suites. This test uses a special microscope (called a colposcope) to examine the cervix and determine whether treatment is necessary. If treatment is required a simple procedure is all that is usually required to remove any abnormal cells. This is done with a thin wire loop (a LLETZ procedure).

An abnormal cyst or tumour can commonly arise from the ovaries or uterus and may cause pelvic symptoms such as pain and discomfort. Your GP may initially investigate these symptoms by arranging for you to have a pelvic ultrasound and some specialised blood tests.
An ovarian cyst may be a simple cyst (almost always benign or non cancerous), or a complex cyst (a cyst with more concerning features that may sometimes have borderline or cancerous changes). In many cases surgical removal of the cyst is the only way to determine whether a cyst is benign, borderline or cancerous.
Fibroids, which are benign tumours in the uterus, are another common problem. When detected, they may not cause women any symptoms or may cause problems such as pelvic pain/discomfort, abnormal bowel or bladder function, pain during intercourse, or abnormal uterine bleeding. Treatment with medication is often effective for fibroids. In situations where medications don’t work, surgery (including hysterectomy i.e. removal of the uterus) may be considered. Minimally invasive options may be possible.
Less frequently, a mass in the uterus can be caused by a cancer. If you have worrisome symptoms or high risk features, Dr Goulding and Dr Green will see you promptly for investigation and treatment.
Use the following links to find detailed information specific to your upcoming surgical procedure:
For more information about specific conditions or tests, click on the links below to access the latest high quality information written specifically for patients:
Cervical Screening
Cervical cancer
HPV vaccination
gestational trophoblastic disease
Fallopian tube cancer
Ovarian cancer
Uterine and endometrial cancer
Endometrial hyperplasia
Vaginal cancer
Vulval cancer
Managing The Ovaries At The Time Of Hysterectomy For Non Cancerous Disease
Fibroids
Menopause
Women’s health (all conditions)
Contraception
Australian Professional Gynaecologic Oncology groups and Research groups: